Medicaid Unwinding and MassHealth Redeterminations
In March 2020, the federal government declared a public health emergency (PHE) due to the COVID-19 pandemic. In response to the PHE and consistent with federal requirements, MassHealth put protections in place that prevented members’ MassHealth coverage ending during the COVID-19 emergency.
The federal government ended its protections and continuous coverage requirements on April 1, 2023. MassHealth has begun a process with members to see if they still qualify for their current MassHealth coverage and benefits. These renewals will take place over 12 months, from April 2023 to April 2024. This means that members could get their renewal forms in the mail at any time during this one-year period. If you or your loved one receives SSI, they most likely will not have to go through the redetermination process.
In order to reduce the number of qualified members that lose their coverage, MassHealth is working with the Massachusetts Health Connector, Health Care For All, and other partners to make sure members know how to renew their coverage and know of other affordable health coverage options if needed.
This redetermination process will be the single largest health coverage transition event since the first open enrollment of the Affordable Care Act and the Medicaid expansion. Most members will either remain eligible for MassHealth or qualify for subsidies that will allow them to get affordable coverage through the Health Connector or other sources.
MassHealth communications have been expanded to include both text and email capabilities. Members who have shared their cell phone number and/or email with MassHealth will receive a text and/or email letting them know their renewal form is coming soon. Renewal forms will be sent to members in a blue envelope. It is essential that MassHealth be given your most recent address.
Related Webinars
Michael Andrade – January 2023 – Preparing for Redetermination
Michael Andrade – February 2023 – Addressing Asset Limits for Redetermination
Vicky Pulos – May 2023 – Redetermination and Key Facts
Resources
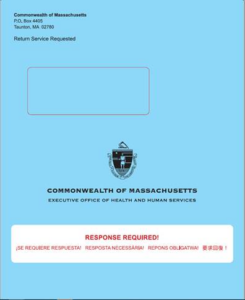 The Blue Envelope and Other Important Mail from MassHealth
The Blue Envelope and Other Important Mail from MassHealth
During the redetermination process, MassHealth will be sending out all renewals to members in a blue envelope. Inside of each blue envelope members will find the following:
- Their renewal notice, including their renewal deadline,
- An insert about their renewal, and
- A paper renewal form.
Important Steps to Take During Phase Two
- Update your information with MassHealth. Make sure MassHealth has your most up to date address, phone number, and email so you do not miss important information and notices from MassHealth.
- Read all your mail. MassHealth will be sending your renewal form in a blue envelope. Additional important notices or request for information may arrive in white envelopes.
- Respond to MassHealth before the deadline. Your notice will have a deadline. Make sure you fill out and send all needed information to MassHealth by the deadline.
If You Need Assistance
- If you have questions about their MassHealth renewal, you can call MassHealth at 1-(800) 841-2900, TDD/TTY: 711 Hours: Monday-Friday 8 a.m. – 5 p.m.
- Assistance is available in English, Spanish, Portuguese, Mandarin, Vietnamese, Arabic, and Haitian Creole, and members may request translators for any other language.
- MassHealth Enrollment Centers (MECs) At a MassHealth Enrollment Center, members can get help with their application from MassHealth employed eligibility staff in person, virtually, or over the phone. It is highly recommended that members schedule a virtual or phone appointment ahead of time at a MEC as there is limited walk-in availability. You can assist them in scheduling an appointment using this link: www.mass.gov/info-details/schedule-an-appointment-with-a-masshealth-representative or by calling MassHealth Customer Service.
- Certified Application Counselors (CACs) are not employed by MassHealth but are trained by MassHealth and the Massachusetts Health Connector to help people apply for health insurance benefits, enroll in health plans, and maintain insurance coverage. Both people who need help maintaining their MassHealth coverage and people who are no longer eligible for MassHealth can get assistance from CACs. Assistance from a CAC is free but may require an appointment. Members can also go to https://my.mahealthconnector.org/enrollment-assisters to find their nearest CAC.
- Some DDS Family Support Centers are also familiar with the Redetermination process and can be of assistance.